Lumbar Disc Herniation
Time and age can exert a lot of pressure on the spine and its discs. In most cases, herniated discs care caused by sustaining trauma or an injury—for example, an accident—that directly exerts pressure on the disc.
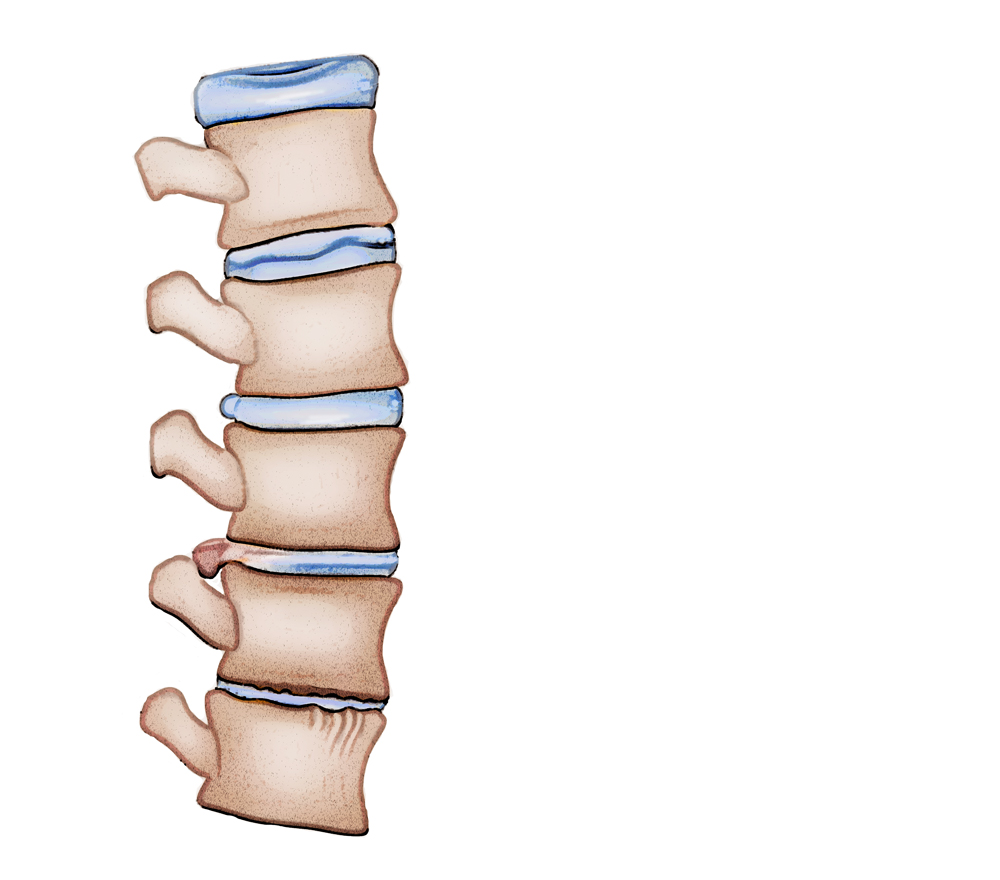
Slowly, over time, the outer bone of the spinal column—called the annulus—cracks and develops tears, causing the gel-like nucleus inside to push out through the tear. This is called a bulging disc.
Bulging discs exert stress on the spinal cord (dura) and the nerve roots that exit through the foramen, extending to the lower limbs and muscles. Symptoms of bulging discs are not always felt.
In case of a weak or brittle annulus, the tears can cause the inner nucleus to protrude (resulting in a ruptured disc) or extrude (resulting in a herniated disc).
Sometimes, the nucleus even leaks fluid and leaves the disc entirely resulting in a condition called a sequestered disc. If left untreated, a herniated disc can progress and increase the pressure exerted on the spinal nerves. This causes inflammation and the resulting pain can either be localized to the lumbar back region or extend down to the limbs and feet.
A herniated disc in the lumbar region is the most common cause of pain the lower back and limbs. Lumbar discs consist of annulus fibrosis, which looks like an interwoven fabric, and the gel-like nucleus pulposus. Placed at each level of the vertebral column, these discs act as shock absorbers.
Herniated Discs: Its Causes
As we age, our spine and discs deal with additional pressure. Most cases of herniated discs stem from experiencing serious physical trauma—for example, an accident—that causes direct pressure in the area the disc is located.
If this compression is left untreated, over time, the annulus will start to develop cracks and tears, causing the inner nucleus to be pushed out and leak fluid through the disc.
This pushing out of the nucleus exerts causes stress to the spinal cord and puts pressure on the nerve roots exiting through the foramen (holes at each level of the vertebral column) and connect with the muscles traveling down your leg.
The pressure exerted combined with the fluid leakage of the nucleus results in inflammation and the resulting pain may most commonly be localized to the back, buttocks, thighs; other times, it may also travel down and extend to the feet.
Risk factors associated with herniated discs are listed in the following:
Aging:
Age causes the discs to wear out and get dry over time, resulting in loss of support and function.
Lifestyle:
Poor lifestyle choices like smoking, lack of a balanced diet, not exercising enough, and obesity attribute to a higher risk of disc degeneration.
Posture:
Maintaining a poor posture when lifting or moving around exerts direct stress and pressure on the spinal and discs.
In the event of conservative treatment failing, the patient will be required to undergo diagnostic tests like CT scans or MRI.
If a neurological deficit is detected, surgical intervention will be recommended. Following are the best surgical treatment options for herniated discs with a success rate of 90%:
- A dull, sharp pain the lumbar regions of the back that worsens with certain physical activities that include lifting heavy objects and bending awkwardly. The pain can also get worse with simple activities like sneezing and conditions like muscle spasms or experiencing muscle cramps.
- Having a condition called sciatica or its symptoms are also often signs of a herniated disc.
- Weakness or loss of function of the leg
Diagnosis
The first step to coming up with an effective treatment plan is a correct and accurate diagnosis.
Here are some of the most effective ways to diagnose the problem areas.
Medical History:
This involves a certified doctor going through a patient’s previous medical and treatment history and assessing symptoms.
Physical Examination:
A spine specialist physically carries out routine spine examination steps to check for problem areas like limitation of movement, balance problems and pain. A thorough spine examination also covers loss of reflexes in extreme regions, weakness in the muscles, loss of sensation or any signs of damage in the spinal cord.
Diagnostic Tests:
This step generally begins with a plain X-ray which helps spine specialists rule out some problems like infections, if required, CT scans and MRIs are then ordered to provide a more detailed three-dimensional view of the lumbar spine which helps detect the presence of herniated discs.
Treatment Options
Disc herniation in the lower spine typically does not warrant surgery. Most often, any pain that stems from a herniated disc heals on its own within 4–6 months without surgical intervention, which is why as a first step, non-surgical treatments are advised to help deal with the symptoms and pain.
Non-Operative Treatment
- Pain meds: anti-inflammatory medication, muscle relaxers and rarely, narcotic painkillers may also be prescribed.
- Administering heat/cold therapy, alternatively, in the first 24–48 hours.
- Helpful and light physical therapy including exercises like stretching, massage strengthening.
- Epidural steroid injections that work to reduce inflammation and determine the level at which the individual experiences pain.
Surgical Treatment for Disc Herniation
In case non-operative treatment doesn’t work and the symptoms persist, the patient is sent for further diagnostic tests like CT scan, MRI or X-ray to identify defects, problem areas or neurological issues.
In case a problem worthy of surgical treatment is detected, the patient is recommended surgical solutions.
In the following are surgical treatment options for the treatment of herniated discs with a success rate of 90%
Microdiscectomy:
This is generally an open procedure where a tubular retractor is used to make an incision of around 1 inch. This is done under anesthesia.
During the procedure, the surgeon uses a microscope or eyeglass loops to observe the area being treated. This procedure has a longer recovery time and the patient might experience some pain from time to time. Most of the pain will come post-operation and is the result of the approach of treatment.
Laminectomy:
Also known as decompression surgery, this process is used to create space for the removal of pressure on a nerve by removing the lamina, the back part of the vertebra, covering the spinal canal.
This procedure is sometimes carried out along with microdiscectomy, and increases the chances of scarring in the area being treated. It also adds to the recovery time.
Endoscopic Discectomy:
This procedure requires an incision of less than half an inch. The process of endoscopic discectomy makes it possible for the surgeon to avoid resection of the lamina bone for entering the spinal canal. It makes it easier to enter the spinal canal without causing major damage including the cutting or disturbing of muscles.
During the procedure, the surgeon is able to observe the herniated disc directly in a water environment (arthroscopy).
To perform the process, a surgical working channel endoscope is used with an HD camera. This procedure requires a comparatively lower recovery time than microdiscectomy, and in most cases, patients are able to return to work in less than a week.
Spinal Fusion
Usually, spine fusion is seen as a last resort for patients displaying symptoms of discogenic back pain or herniated discs.
The process of endoscopic discectomy allows physicians to detect the affected disc while the patient is under conscious sedation.
The procedure involves making an incision of around ¼ of an inch and placing a 7 mm working cannula into the foramen. This insertion is usually done from the side to avoid causing any major damage to the surrounding muscles or tissues.
An HD camera is then guided into the working channel endoscope to help the physician carry out the procedure accurately.
Recovery
At our practice, many patients who undergo spinal fusion will be able to get out of bed in just over an hour of the having the procedure performed and will be able to go home shortly afterward.
There is some pain, localized to the incision site, that will be felt from time to time for a few days, post-surgery, but despite that fact, most people will feel well enough to return to work in a few days. Till then, pain killers will be provided to ease the post-op symptoms.
Once you’re done with the procedure, plenty of rest is recommended to speed up the healing process. The doctors will make sure to provide you with ample guidance on how to care of your area of incision and gradually increase physical activity to not set back the recovery time and avoid any further damage to the area of treatment.
The pain and discomfort will begin to heal in a couple of days post-surgery and patients will be instructed to use adequate medication and techniques for reducing pain and increasing flexibility.
The patient will also be given a time frame to indicate when and how to resume daily activities such as walking, lifting weight and driving and the optimal time frame of returning to activities like physical labor work or sports.
