Facet Syndrome
Facet joint syndrome or chronic axial back pain may result in chronic pain or severe spasms in the neck and back region that worsens with physical activities like walking, standing, leaning backward or bending over. If you’re experiencing any of these symptoms, you may be suffering from one of these conditions.
Facet Joint Syndrome
Progressing age causes wear and tear in the structures of the spine. This wear and tear sometimes develops into a condition called facet syndrome, which is one of the most common types of arthritis.
Even though this is commonly seen in the elderly population—usually comprising of adults aged over 50 years—it may also develop in younger people.
However, the causes of the condition in young people are most commonly physical trauma or overuse of the backbone.
Every day, hundreds of Americans deal with these conditions, adopting ways and methods to manage the symptoms with lifestyle changes so that they don’t have to go for surgery.
At Houston Neurosurgery and Spine, we make it a point to get an extensive and thorough history of your health and symptoms before making a diagnosis and moving on to further treatment.
We also use diagnostic imaging and special injections to detect if a facet joint is the cause of pain. If a facet joint is found to be linked to the pain, the patient is referred to an interventional pain physician who can treat the pain using non-surgical methods.
Facet Joint Syndrome: The Causes
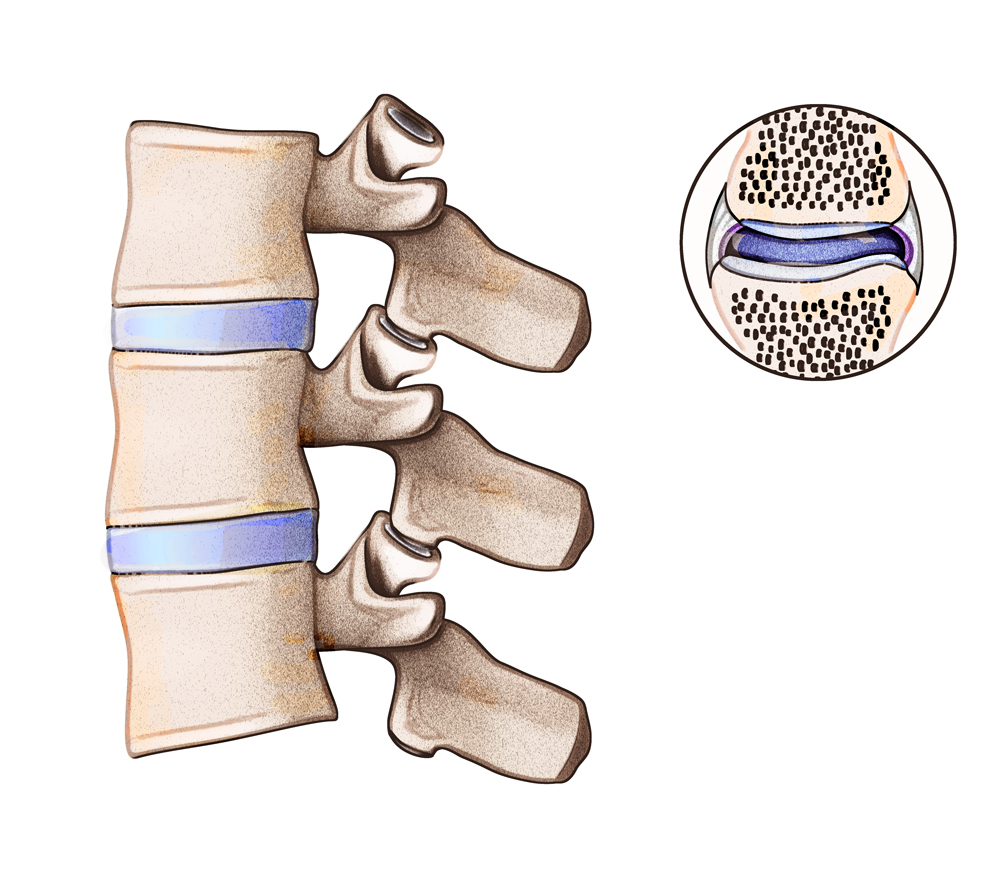
Facet joints are small joints, placed between each individual vertebra in the vertebral column. These joints are lined with cartilage, providing the necessary lubrication in order to provide the spine the needed flexibility. This cartilage helps the joints maintain their function of constant motion, allowing us to carry out physical activities like walking, bending, and twisting.
Sometimes, due to injury, overuse or aging, the cartilage inside the facet joint can break down, wear out and cause growths known as ‘bone spurs’ to develop, creating friction in the joints. This friction can lead to a multitude of issues including swelling, tenderness, pain and stiffness.
Damage to the joint like injury, deterioration or any kind of physical trauma may result in swelling, pain and stiffness. The resulting inflammation may be temporary but having arthritis may complicate the situation and lead to long-term or even permanent disability.
There are additional risk factors for the facet syndrome apart from age. These include:
- Obesity
- Overuse of the spinal column in an improper posture for sports or heavy labor
- Having certain medical conditions like gout, arthritis or infections
- Physical trauma like injuries or excessive weight lifting in an improper posture
- Pain that is aggravated in the morning and at night or is affected by climate changes.
- Radiating pain in the lumbar back region that spreads to the shoulders, one or both arms and sometimes even the hands
- Ringing in ears that is accompanied by a headache at the back of the head, the base of the skull or behind the eyes.
- Muscle weakness in limbs
- Lower back pain after standing for a long time
- Pain that worsens on sitting for a long time
Symptoms of facet joint syndrome or axial back pain can be managed and reduced to a great extent without surgical intervention. The degree of relief felt differs from patient to patient and ranges from temporary to significant.
- Physiotherapy that would help support the core muscles and strengthen your back to improve posture.
- Alternating between hot and cold compresses
- NSAID (non-steroidal anti-inflammatory medication, such as ibuprofen) and COX-2 inhibitors (such as Celebrex)
- Lifestyle changes that would help reduce pressure on the muscles at the back
Sometimes, conservative care doesn’t work and the symptoms progress and become chronic.
If this continues for a period of more than six months, surgical intervention or injections may be required to help ease the symptoms. The facet joints connect to the exiting nerve through a small medial branch nerve that connects to the column of muscles in the back. This is the nerve that carries the pain signals from the back to the brain.
A pain management physician can easily diagnose this condition with the help of a series of examinations like a physical check-up, radiographic readings, and finally, a confirmatory facet medial branch block injection. If the pain relief experienced is rated to be higher than 90%, the patient may be recommended a percutaneous radio frequency rhizotomy.
The percutaneous rhizotomy procedure consists of a probe being inserted into the body, guided by an X-ray image, allowing indirect visualization for targeting the medial branch nerve.
Next, the probe is heated to help ablate the small nerve, resulting in instant pain relief.
According to patient reviews, a percutaneous rhizotomy successfully resolves pain related issues in about 70% of patients who opt for it for a year. In some cases, the results may even last up to 5 years. It is up to the patient to choose to be sedated or not, depending on their pain threshold.
When percutaneous radio frequency doesn’t seem to be helping, or the effect fades off too quickly, an endoscopically assisted radio frequency rhizotomy might help. To carry out the procedure, a 7mm tube is inserted into the facet, assisted by X-ray imaging and a working channel endoscope tube attached to an HD camera.
Guided by direct visualization, a physician is able to ablate the medial branch nerve with a radio frequency probe. According to results from clinical literature, around 80% of patients reported a 50% or more reduction in back pain which lasted for up to 5 years. The endoscopic approach has also proven to last longer than radio frequency ablation.
