One of the most common, yet the most misunderstood causes of lower back pain, is degenerative disc disease.
This degenerative condition in the lower regions of the back indicates that one or more of the discs in your vertebral column have become dehydrated and have started to deteriorate, resulting in pain in the lumbar back.
In some case, this condition can occur as a result of genetics; in other, more common cases, developing this condition may have multiple reasons.
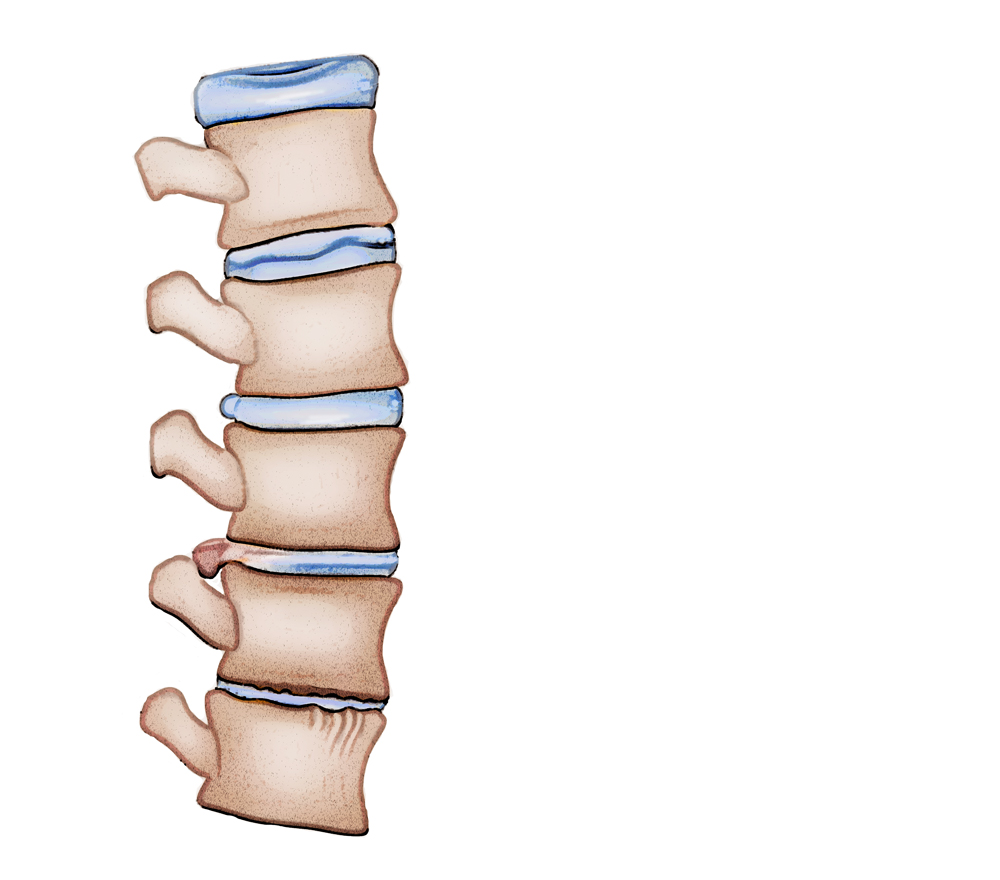
Your spinal discs act as shock absorbers between the bones in your spine called vertebrae. Your disc and spine work together to help you turn, twist, bend and stay flexible.
As you get older, the disc can show signs of wear and tear. They begin to break down and may not work as well.
Over time and as we age, our vertebrae and the discs located within can wear and develop micro tears in its outer wall. This outer wall is called the annulus. Apart from age, this condition can also occur as a result of physical trauma for example an injury, an accident or another physical activity such as lifting heavy objects improperly.
The spinal discs do not get sufficient blood supply, so in the case of injury or sustaining physical trauma, they are unable to repair themselves.
Sometimes, direct damage to the disc can set off a cycle of degeneration and the disc starts to deteriorate. The degenerative disc disease is a common problem and affects an approximate of 30% of people between 30–-55 years of age.
Even though one of the symptoms of the degenerative disc disease is pain, not every person diagnosed with the condition will experience it. Most people won’t even be diagnosed with it. However, it is common for people over the age of 60 to have some level of disc degeneration that are easily indicated on MRI scans.
As we age, so does our spine. One of the most common, yet the most misunderstood causes for neck and lower back and neck pain is the degenerative disc disease.
One or more of the discs in our spinal columns become weak and dehydrated and start deteriorating, resulting in pain in the lumbar regions of the back. This condition is called the degenerative disc disease.
Although the most common causes of this condition include aging and suffering from physical trauma like an accident or an injury which causes the discs to wear down and develop micro tears in the annulus (the outer wall of the disc), it can also stem from a genetic background.
The discs in our spine cannot repair themselves because they are not connected to any means of blood supply. This is why sometimes, a simply injury or an accident can set off a cycle of degenerative damage that wears out the disc and makes it weaker. This condition is fairly common, affecting around 30% of people aged between 30–50 years.
Even though it is normal and expected to find a certain level of disc degeneration in the MRI scans of elderly patients, not all people experiencing this condition will have pain symptoms or even reach a formal diagnosis.
Annular Tears or Disc Tears
Physical impact, trauma, injury, accidents or even aging can cause the outer layers of the disc to develop tears.
This exposes the spinal nerves and the inner nerves to the gel-like nucleus pulposus and results in extreme pain. If the annular tear is left untreated, it can enlarge and result in disc herniation.
The most accurate way to diagnose or detect annular tears is by reviewing a patient’s pain history and observing MRI scans where the tears are shown as white, high intensity zones on the posterior discs. The pain that is experienced as a result of having annular tears is called discogenic pain.
What Causes Annular Or Disc Tears?
With trauma, degeneration begins and the outer layers of the disc may tear (Annular Tear) and may expose the spinal nerve and exiting nerve to the inner nucleus pulposus. It is believed that nucleus pulposus can irritate one or both of the nerves and thus produce a great deal of pain. If the annular tear becomes large enough the disc may protrude, extrude or herniate through the tear resulting in a disc herniation. Annular tears can be diagnosed with a history of pain and can be observed on an MRI as a white, high intensity zone on the posterior disc. Discogenic pain is the term used to describe pain resulting from annular tears.
- Excessive weight
- Overuse due to sports or heavy labor
- Presence of disease such as gout, other types of arthritis, or infections
- Damage may stem from injuries or trauma, including whiplash,
- Excessive lifting of heavy weight
- Pain in the lumbar regions of the back, around the affected area. This kind of pain usually radiates down to the thighs but does not go past the knees.
- A numbing sensation or tightness around the affected area may indicate the presence of tears in the disc or disc herniation
- Numbness in arms or legs may sometimes be a result of bulging or herniated discs as they compress the spinal nerves.
- Pressure on the spinal nerves may also result in weakness in their limbs leading to problems like losing grip or temporary loss of control.
A tingling sensation in hands or feet
- Medical history
Assessment of symptoms, previous treatments and care. - Physical examination.
A careful examination by a spine specialist for limitations of movement, problems with balance, and pain. The examination should also cover loss of reflexes in your extremities, muscle weakness, loss of sensation or signs of spinal cord damage. - Diagnostic tests.
Generally, we start with plain x-ray films, which allow us to rule out other problems such as infections. CT scans and MRIs are often used to give us three-dimensional views of the lumbar spine and can help detect herniated discs.
Treatment Options
In case disc herniation is not found, the following conservative treatments may be considered:
- Alternating heat or cold therapy
- Lifestyle changes and exercise
- Epidural steroid injections
- Non-steroidal anti-inflammatory pain medicines
- Professional physiotherapy and regular massages in the affected area
- Transcutaneous electrical nerve stimulation
Surgical Treatment
If conservative treatment doesn’t seem to be working even 6 months post administration and there is no pain relief, an open Endoscopically Assisted Tubular Retractor Surgery is recommended.
Clinical literature suggests that the procedure helps alleviate pain to a very high degree, successfully.
To carry out the procedure an operating tube of approximately 7mm, is placed into a ¼ inch incision in the disc of the affected region.
An endoscope paired with an HD camera is then inserted into the operating tube to visually assist the physician in getting a better look at the inner structures such as the annulus or the spinal nerves.
The tear is then fixed and the nucleus pulpous is enclosed inside the tear with the help of a thermally heated bipolar instrument.
Compression Fracture
Back pain can range from moderate to extremely painful, and one of the back related conditions that can cause excruciating pain is a compression fracture.
However, most people aren’t aware of the fact that a simple six-minute procedure called Kyphoplasty can eliminate the majority of the pain immediately.
The procedure consists of filling the fractures and cracks with epoxy/cement. When the material hardens, it will provide the necessary bone support and alleviate the pain caused by bone movement. The alternative is to take pain medication.
What Is The Recovery ?
Most patients can begin getting out of bed one hour after surgery and go home shortly afterwards. With a spine fusion the time for post-operative recovery is much longer and may involve overnight stay in the hospital. Activity is gradually increased and patients are typically able to return to work within a few days. With a spine fusion return to work may be upto 2 months. There will probably be some pain after the procedure and is usually localized to the incision site. However, just because there is less or no pain, always consult your physician before beginning any physical work.
At home, you will need to continue to rest. You will be instructed on how to gradually increase your activity. You may still need to take the pain medications for a while. However, pain and discomfort should begin to reduce within a couple of days after surgery. The doctor will discuss with you other techniques for reducing pain and increasing flexibility before you leave for home. The doctor will also discuss with you a time frame for when you can resume basic activities such as walking, driving and light lifting, and when you can return to more advanced activities such as physical labor, sports and yard work.
