LET US HELP.
Request An Appointment TodayDo you have questions?
Call us. (832) 522-8500
Back Pain Surgery
Causes |
How Your Back Works And Why It Hurts
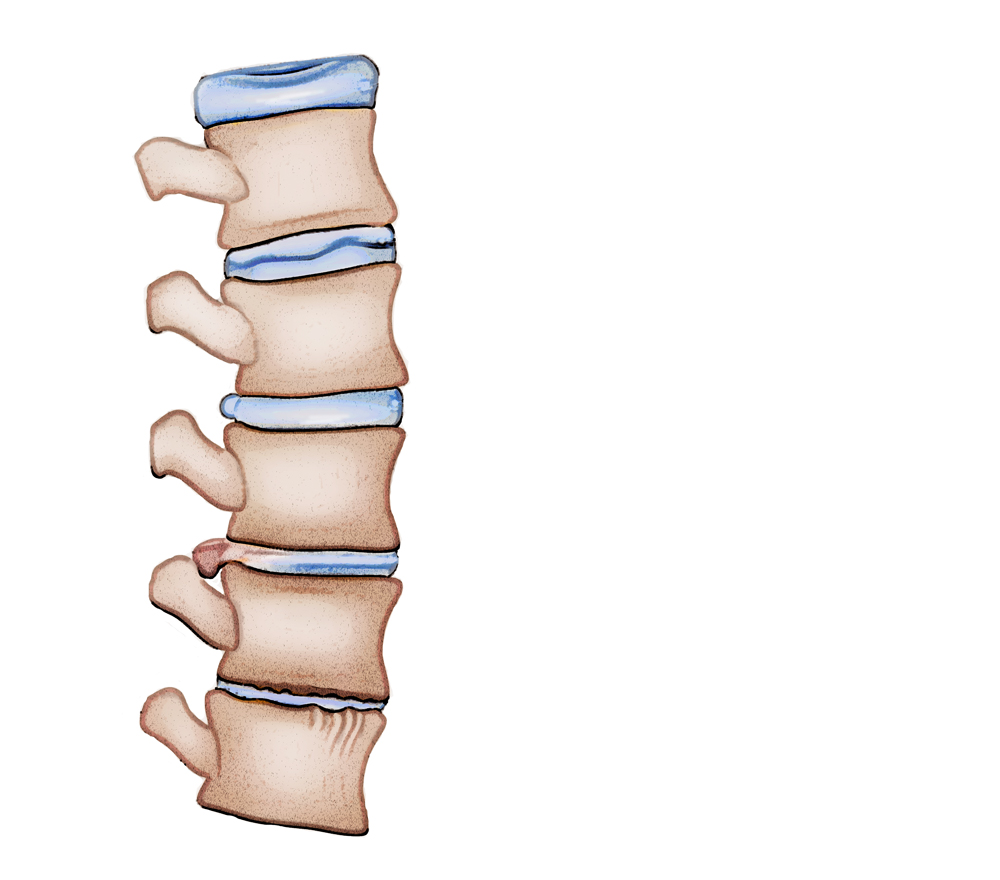
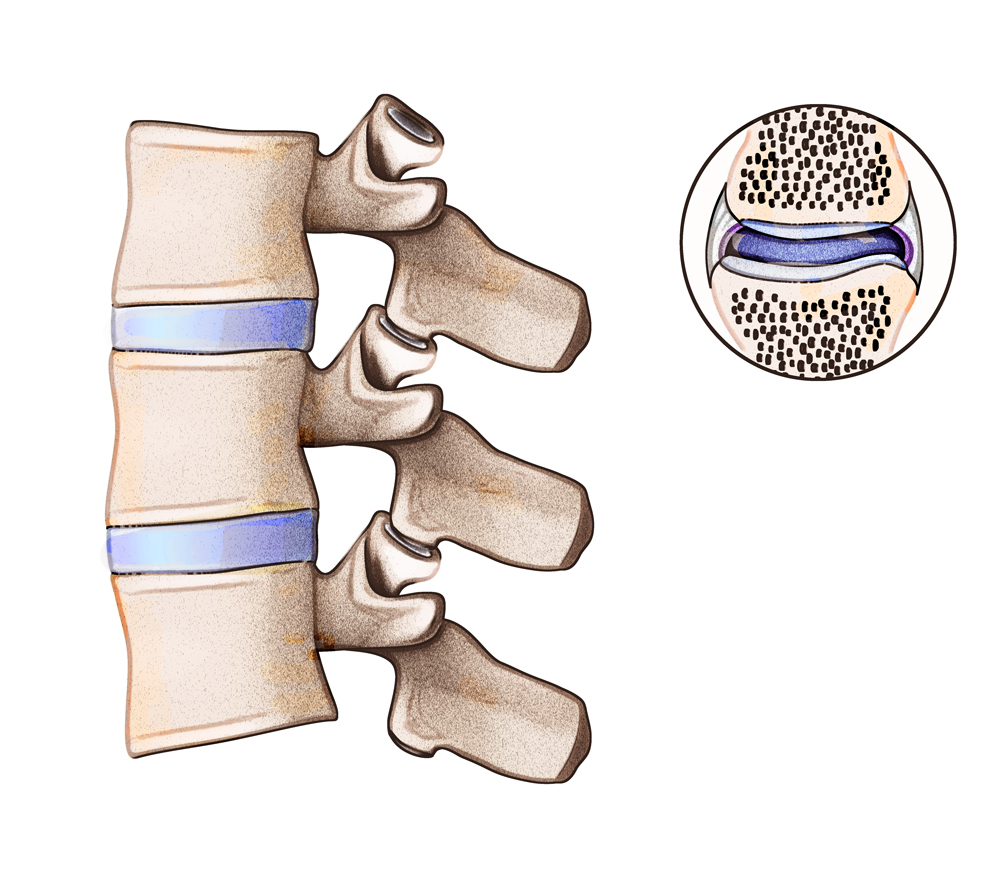
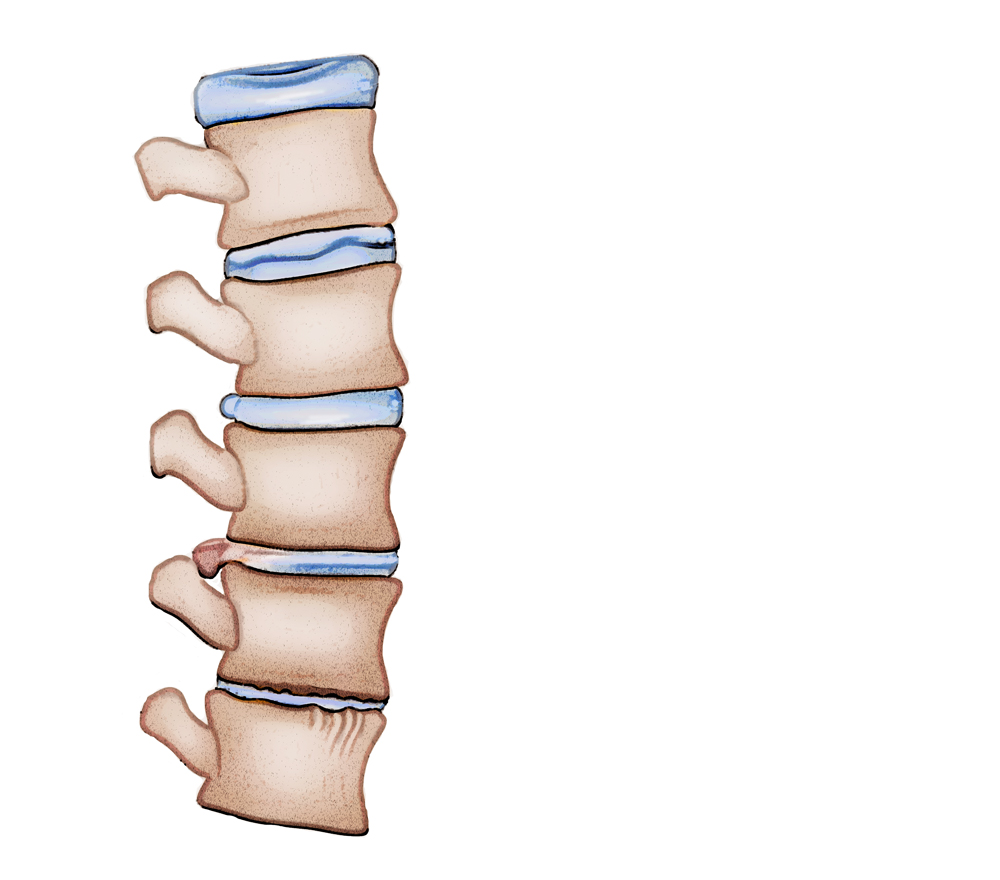
Your spinal column—or vertebrae—is comprised of 33 bones that support your entire body.  Aside from protecting your spinal cord, it allows you to stand and sit upright as well as walk, bend, and twist. The bones in your vertebrae sit one on top of another, and are surrounded by supporting ligaments and muscles. They are separated by discs that act as shock absorbers between the bones to keep the vertebrae flexible.
Aside from protecting your spinal cord, it allows you to stand and sit upright as well as walk, bend, and twist. The bones in your vertebrae sit one on top of another, and are surrounded by supporting ligaments and muscles. They are separated by discs that act as shock absorbers between the bones to keep the vertebrae flexible.
The spinal cord—a long, thin structure that is made of nervous tissue—passes through the vertebrae, connecting the brain to the rest of the body. It joins the brain at the base of the skull and houses a system of nerves that pass through the spaces between the bones of the spine.
There are several factors that cause back pain, such as poor posture, a lack of exercise, or muscle strains or sprains. As you age, the structures that hold the spine together start to lose their flexibility and integrity causing back back and other underlying issues.
Serious Causes Of Back Pain And Treatment Options—The Best Care In Houston
Sciatica is a leading cause of back and spine pain. The bulging or herniated disc pinches or compressing a nerve causing back pain that extends to your legs. You may also feel numbness and tingling with sciatica.
As the back or spinal pain pain progresses, you know how difficult it can be to carry out daily activities including going to work or playing with your children.
After a thorough screening which may include CT scans, MRIs, or X-rays, you may be able to relive your sciatica pain through physiotherapy or other non-invasive treatments. In many cases, the pain diminishes within four to six months without surgery. However, if the pain persists and becomes intolerable, your may need consider surgery, as your best option to relieve the pressure and pain on your spine.
At Houston Neurosurgery & Spine, we understands how debilitating pain caused by sciatica can be. That’s why you’ll find a range of non-operative and minimally-invasive surgical solutions in Houston for treating back pain, lower back pain, neck pain, herniated discs, sciatica and bulging discs in the lower back.
Schedule a appointment to see world-renowned neurosurgeon, Dr. G. Alexander West, for a thorough assessment of your condition.
For expert medical care, visit our clinic in Houston, Texas.
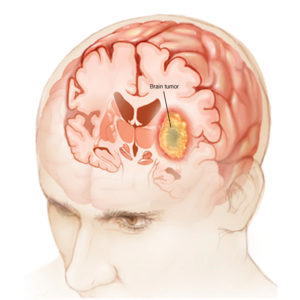
Brain and Spinal Tumors
Tumors in the central nervous system (CNS) range from benign to malignant. While benign tumors are noncancerous and do not spread, malignant tumors are cancerous and have spread or will eventually spread.
Since benign tumors are well defined with visible boundaries and grow slowly, surgical methods can help. Abnormal growths like tumors in our CNS are painful because the growths push nerves against bony appendages, causing pain. This impairs tissue function as well.
Knowing the tumor’s origin can provide some relief. Tumors that originate in the CNS itself are primary tumors that are either hereditary or they develop from abnormal and excessive cell growth on surrounding nerves. Additionally, radioactive rays and chemicals can also cause primary tumors.
Tumors that originate elsewhere in the body are called metastatic tumors. These indicate that some other body part has extracted cancer cells and growth—most commonly in the lungs.
What Are The Symptoms of Brain and Spinal Tumors
Brain and spine tumor symptoms are wide-ranging and include:
- Nausea
- Vomiting
- Impaired vision
- Impaired hearing
- Seizures
- Headaches
- Loss of balance
- Impaired motor functions and skills
- Weakened cognition
- Behavioral issues
- Weakness and fatigue
- Issues in the bladder and bowels
- Extremity sensation loss
How Is A Brain and Spinal Tumors Diagnosed?
At Houston Neurosurgery & Spine, we diagnose brain and spine tumors through neurological examination, special imaging, or other testing procedures that may include:
- MRI (magnetic resonance imaging)
- CT scan (computed tomography)
- PET scan (positron-emission tomography)
- EEG (electroencephalogram)
- Spinal tap
Kinds of Brain and Spine Tumor
Some of the common brain and spine tumors include:
- Glioblastoma multiforme (GBM)
- Meningiomas
- Acoustic neuromas
- Pituitary adenomas
- Cranial extensions of head and neck cancers
What Are The Treatment Options For A Brain and Spinal Tumors
Tumor Removal and Craniotomy
Our surgeons may perform a craniotomy procedure to remove some tumors. We find that this is especially effective in treating benign tumors.
Using high-tech intraoperative images to guide us, we employ a minimal access neurosurgical approach to ensure that the incisions made are as minuscule as possible.
Surgical safety and precision matter most to us. For example, we use real-time intraoperative MRI for optimal precision and to reduce the risk of the tumor spreading.
Our minimal access approaches help us increase our surgical precision, minimize our patient’s hospital stay, and allow our patients to recover much faster.
Neuroendoscopy
Neuroendoscopy is a surgical procedure where tumors in far-reaching and deep regions in the brain and the cranium are removed through small, dime-sized holes in the patient’s skull or through the mouth or nose. As an alternative to traditional surgery, this surgical approach uses endoscopes and surgical microscopes so the incision site is minute. Neuroendoscopy also creates minimal trauma to surrounding tissues, shortening the patient’s hospital stay.
Cervical Myelopathy
The compression of nerves in the neck is called cervical myelopathy. The additional pressure results in impaired motor skills, stiff neck, mild to severe pain, loss of balance, and troubled gait.
MRI is the most common way to diagnose cervical myelopathy, and in most cases, Spine Decompression Surgery is the most effective way to treat it.
What Causes A Cervical Myelopathy
The spine consists of 33 vertebrae, out of which 7 are present in the cervical region, along with 8 nerve roots and 6 interverbal discs. The spinal cord—the soft cord that is the backbone of all the brain’s commands and instructions—is protected inside of this bony structure.
When the spinal cord in the cervical region becomes compressed, the condition is called cervical myelopathy. Since the spinal cord is essential for the brain’s control of your motor skills and gait, they naturally get affected.
While aging and gradual spinal degeneration can cause cervical myelopathy, there are other conditions that can cause this condition:
- Ossification: Patients experience hardening of the ligaments—most commonly, the posterior ligaments—around the spinal region. This is where the soft tissue that connects vertebra to vertebra undergoes bone tissue formation, causing friction and pain. As the hard bone gradually grows, it creates pressure on the nerves.
- Other causes include rheumatoid arthritis in the neck, infections in the spine, spine trauma, whiplash, cancer or tumors in the spine
What Are The Symptoms of Cervical Myelopathy
Although cervical myelopathy originates in the neck, where you’ll experience much pain, other symptoms can also indicate cervical myelopathy. These usually occur below the cervical region, where the nerves are compressed.
Symptoms in the neck include:
- Mild to severe pain
- Not being able to move your neck
- Stiff neck
Additionally, if the condition progresses unchecked, patients experience sharp pains that originate in the cervical region and travel down to other parts of the spine.
Other symptoms that don’t materialize in the neck include:
- Weakness in the limbs
- Clumsiness
- Poor coordination of limbs
- Problems in maintaining balance
- Inability to handle minute objects such as pencils and knives
- Numb fingers accompanied by tingling
If you’re experiencing neck pain, consult with a doctor to ensure it’s not muscular pain.
Cervical Spondylotic Myelopathy
As we age above 50 years old, our spinal canal narrows and the spine degenerates, causing Cervical Spondylotic Myelopathy.
Additionally, people who have narrow spinal canals may experience Cervical Spondylotic Myelopathy earlier than usual. Other causes may include herniated discs, bulging in the neck, and bone spurs.
How Is A Cervical Myelopathy Diagnosed?
Early diagnosis is the key to finding effective relief from cervical myelopathy. A regular diagnosis at Houston Neurosurgery & Spine includes:
- Physical examination accompanied by measurement of muscle strength and evaluation of reflexes
- Tests that include: MRI, CT scan, X-rays, myelogram
- Electrical tests for the determination of how well nerves in the limbs are communicating and coordination with the brain.
What Are The Treatment Options For A Cervical Myelopathy
Depending on the severity of the condition, you can undergo surgical or non-surgical treatments for cervical myelopathy.
Non-Surgical Treatments
- Physical therapy
- Collar brace
Spine Fusion
Surgeons can operate on your spine to join multiple bones in the spine for relief from cervical myelopathy. The spinal cord is made up of vertebrae, each separated and cushioned by intervertebral discs, and the soft spinal cord lies inside.
Conditions such as arthritis cause these intervertebral discs to stop cushioning, causing the vertebrae to move abnormally or against each other, resulting in pain, immobility, etc.
In spine fusion, our surgeons substitute the intervertebral discs with bone-like grafts. At Houston Neurosurgery & Spine, we perform minimally invasive spine fusion, with a small incision under anesthesia so your recovery time is considerably shorter as compared to traditional surgeries.
Surgical Treatment
For complete elimination of the problem and the prevention of its worsening, surgery is recommended. These include:
- Laminoplasty
- Decompression surgery
- Spine fusion.
Surgeons operate anteriorly or posteriorly through the neck depending on the particular condition.
Recovery
You might experience neck pain in the weeks following the surgery. Many patients say that they can’t sit or stand in the same position for long periods and need pain medication to manage the discomfort. Physiotherapy is often recommended to restore limb mobility and help strengthen your muscles. You will fully recover from the surgery after 8 weeks.
Book an appointment with Houston Neurosurgery & Spine for a complete diagnosis and prognosis.
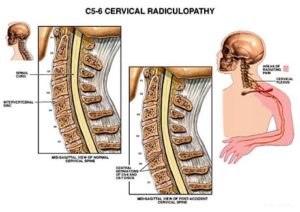
Cervical Radiculopathy
What Causes A Cervical Radiculopathy
Radiculopathy happens when other medical conditions cause pressure on the spinal nerves.
These conditions are:
Herniated Disc
Disc Herniation occurs because of erosion in the spinal disc, which allows the inner annulus to enter the spinal canal. The escaped tissue presses on the nerves in the spinal canal to cause radiculopathy.
Scoliosis
A spine that curves sideways is called scoliosis. Scoliosis might cause radiculopathy because abnormal spine curvature can pinch the nerves in your spine.
Diabetes
Diabetes can cause radiculopathy by reducing blood supply to the nerves in the spine.
Other Causes
Other medical conditions that cause radiculopathy include spinal tumors, sciatica, osteoarthritis, and bone spurs.
What Are The Symptoms of Cervical Radiculopathy
People with radiculopathy often report the following symptoms:
- Back pain or pain in the shoulders, arms, or legs. Pain from radiculopathy might get worse if you cough, sneeze, or engage in physical activity.
- Weakness in the limbs and slower reflexes.
- Numbness, tingling or oversensitivity in the limbs.
Your symptoms will vary, depending on the type of radiculopathy you have. Your doctor will conduct a thorough diagnostic assessment to determine which nerve is pinched and causing your symptoms.
How Is A Cervical Radiculopathy Diagnosed?
The doctor will conduct a physical examination to determine the site affected by radiculopathy. The physical examination includes the following tests:
- X-ray
- MRI
- CT scan
What Are The Treatment Options For A Cervical Radiculopathy?
Radiculopathy can be treated by two methods:
- Medication
- Surgery
Medication
In most cases, over-the-counter drugs like ibuprofen, acetaminophen, etc. can provide pain relief. Doctors may also prescribe steroids if needed. Medication is a conservative, but no less effective treatment for radiculopathy.
However, if your case is severe and nerve damage is advanced, your neurologist could suggest surgery.
Surgical Treatment
Through surgery, doctors operate on the spinal disc and the herniated disc to relieve the pressure on compressed nerves.
At Houston Neurosurgery &Spine, we employ noninvasive surgical methods to provide relief from compressed nerves and the corresponding pain. These surgical methods include:
Arthroplasty
Arthroplasty involves replacing the disc in the cervical spine using microscopic technology. Here, we locate the pain’s exact origin by entering through the front of the neck.
Once the pain is pinpointed, we replace the natural, dysfunctional disc with a synthetic disc that functions as a healthy one. The surgery lasts from an hour to1.5 hours, and the results are seen fairly quickly.
Posterior Cervical Foraminotomy
Posterior cervical foraminotomy is an outpatient surgical procedure performed while the patient is under anesthesia. This procedure involves surgically removing the compressed nerves in the spine and vertebral region.
Lumbar Microdiscectomy
Lumbar microdiscectomy is a minimal access surgical approach that reduces open-surgery related trauma. The surgery has shorter recovery times and results in less scarring and negligible post-surgery pain. This minimally invasive surgery removes bulges from the herniated region, providing pain relief from compressed nerves.
Using X-ray technology to pinpoint the pain’s origin, surgeons monitor the procedure with a microscope and use a retractor tube to remove the bulge. Once the nerve is free, the retractor tube is pulled out, and the incision is closed using plastic surgical methods to hide the incision. Lumbar microdiscectomy is highly effective, and patients are able to walk easily within 24 hours of the surgery.
Recovery
You might have to stay in the hospital for up to 2 days after surgery, but you’ll be able to walk or eat by yourself within a day of the procedure. Some patients experience hoarseness or difficulty swallowing if they get surgery for cervical radiculopathy and must wear a rigid cervical collar for a time. You will also have to go for physical therapy to recover limb mobility and muscle strength. You can go back to normal activities 4 to 6 weeks after the surgery.
At Houston Neurosurgery &Spine, we promise minimally invasive surgery that provides long-term pain relief. We take most insurance plans, so book your appointment with us in Houston.
Degenerative Disc Disease
One of the most common, yet the most misunderstood causes of lower back pain, is degenerative disc disease.
This degenerative condition in the lower regions of the back indicates that one or more of the discs in your vertebral column have become dehydrated and have started to deteriorate, resulting in pain in the lumbar back.
In some case, this condition can occur as a result of genetics; in other, more common cases, developing this condition may have multiple reasons.
Your spinal discs act as shock absorbers between the bones in your spine called vertebrae. Your disc and spine work together to help you turn, twist, bend and stay flexible.
As you get older, the disc can show signs of wear and tear. They begin to break down and may not work as well.
Over time and as we age, our vertebrae and the discs located within can wear and develop micro tears in its outer wall. This outer wall is called the annulus. Apart from age, this condition can also occur as a result of physical trauma for example an injury, an accident or another physical activity such as lifting heavy objects improperly.
The spinal discs do not get sufficient blood supply, so in the case of injury or sustaining physical trauma, they are unable to repair themselves.
Sometimes, direct damage to the disc can set off a cycle of degeneration and the disc starts to deteriorate. The degenerative disc disease is a common problem and affects an approximate of 30% of people between 30–-55 years of age.
Even though one of the symptoms of the degenerative disc disease is pain, not every person diagnosed with the condition will experience it. Most people won’t even be diagnosed with it. However, it is common for people over the age of 60 to have some level of disc degeneration that are easily indicated on MRI scans.
As we age, so does our spine. One of the most common, yet the most misunderstood causes for neck and lower back and neck pain is the degenerative disc disease.
One or more of the discs in our spinal columns become weak and dehydrated and start deteriorating, resulting in pain in the lumbar regions of the back. This condition is called the degenerative disc disease.
Although the most common causes of this condition include aging and suffering from physical trauma like an accident or an injury which causes the discs to wear down and develop micro tears in the annulus (the outer wall of the disc), it can also stem from a genetic background.
The discs in our spine cannot repair themselves because they are not connected to any means of blood supply. This is why sometimes, a simply injury or an accident can set off a cycle of degenerative damage that wears out the disc and makes it weaker. This condition is fairly common, affecting around 30% of people aged between 30–50 years.
Even though it is normal and expected to find a certain level of disc degeneration in the MRI scans of elderly patients, not all people experiencing this condition will have pain symptoms or even reach a formal diagnosis.
Annular Tears or Disc Tears
Physical impact, trauma, injury, accidents or even aging can cause the outer layers of the disc to develop tears.
This exposes the spinal nerves and the inner nerves to the gel-like nucleus pulposus and results in extreme pain. If the annular tear is left untreated, it can enlarge and result in disc herniation.
The most accurate way to diagnose or detect annular tears is by reviewing a patient’s pain history and observing MRI scans where the tears are shown as white, high intensity zones on the posterior discs. The pain that is experienced as a result of having annular tears is called discogenic pain.
What Causes Annular Or Disc Tears?
With trauma, degeneration begins and the outer layers of the disc may tear (Annular Tear) and may expose the spinal nerve and exiting nerve to the inner nucleus pulposus. It is believed that nucleus pulposus can irritate one or both of the nerves and thus produce a great deal of pain. If the annular tear becomes large enough the disc may protrude, extrude or herniate through the tear resulting in a disc herniation. Annular tears can be diagnosed with a history of pain and can be observed on an MRI as a white, high intensity zone on the posterior disc. Discogenic pain is the term used to describe pain resulting from annular tears.
- Excessive weight
- Overuse due to sports or heavy labor
- Presence of disease such as gout, other types of arthritis, or infections
- Damage may stem from injuries or trauma, including whiplash,
- Excessive lifting of heavy weight
- Pain in the lumbar regions of the back, around the affected area. This kind of pain usually radiates down to the thighs but does not go past the knees.
- A numbing sensation or tightness around the affected area may indicate the presence of tears in the disc or disc herniation
- Numbness in arms or legs may sometimes be a result of bulging or herniated discs as they compress the spinal nerves.
- Pressure on the spinal nerves may also result in weakness in their limbs leading to problems like losing grip or temporary loss of control.
A tingling sensation in hands or feet
- Medical history
Assessment of symptoms, previous treatments and care. - Physical examination.
A careful examination by a spine specialist for limitations of movement, problems with balance, and pain. The examination should also cover loss of reflexes in your extremities, muscle weakness, loss of sensation or signs of spinal cord damage. - Diagnostic tests.
Generally, we start with plain x-ray films, which allow us to rule out other problems such as infections. CT scans and MRIs are often used to give us three-dimensional views of the lumbar spine and can help detect herniated discs.
Treatment Options
In case disc herniation is not found, the following conservative treatments may be considered:
- Alternating heat or cold therapy
- Lifestyle changes and exercise
- Epidural steroid injections
- Non-steroidal anti-inflammatory pain medicines
- Professional physiotherapy and regular massages in the affected area
- Transcutaneous electrical nerve stimulation
Surgical Treatment
If conservative treatment doesn’t seem to be working even 6 months post administration and there is no pain relief, an open Endoscopically Assisted Tubular Retractor Surgery is recommended.
Clinical literature suggests that the procedure helps alleviate pain to a very high degree, successfully.
To carry out the procedure an operating tube of approximately 7mm, is placed into a ¼ inch incision in the disc of the affected region.
An endoscope paired with an HD camera is then inserted into the operating tube to visually assist the physician in getting a better look at the inner structures such as the annulus or the spinal nerves.
The tear is then fixed and the nucleus pulpous is enclosed inside the tear with the help of a thermally heated bipolar instrument.
Compression Fracture
Back pain can range from moderate to extremely painful, and one of the back related conditions that can cause excruciating pain is a compression fracture.
However, most people aren’t aware of the fact that a simple six-minute procedure called Kyphoplasty can eliminate the majority of the pain immediately.
The procedure consists of filling the fractures and cracks with epoxy/cement. When the material hardens, it will provide the necessary bone support and alleviate the pain caused by bone movement. The alternative is to take pain medication.
What Is The Recovery ?
Most patients can begin getting out of bed one hour after surgery and go home shortly afterwards. With a spine fusion the time for post-operative recovery is much longer and may involve overnight stay in the hospital. Activity is gradually increased and patients are typically able to return to work within a few days. With a spine fusion return to work may be upto 2 months. There will probably be some pain after the procedure and is usually localized to the incision site. However, just because there is less or no pain, always consult your physician before beginning any physical work.
At home, you will need to continue to rest. You will be instructed on how to gradually increase your activity. You may still need to take the pain medications for a while. However, pain and discomfort should begin to reduce within a couple of days after surgery. The doctor will discuss with you other techniques for reducing pain and increasing flexibility before you leave for home. The doctor will also discuss with you a time frame for when you can resume basic activities such as walking, driving and light lifting, and when you can return to more advanced activities such as physical labor, sports and yard work.
Facet Joint Syndrome
Facet Syndrome
Facet joint syndrome or chronic axial back pain may result in chronic pain or severe spasms in the neck and back region that worsens with physical activities like walking, standing, leaning backward or bending over. If you’re experiencing any of these symptoms, you may be suffering from one of these conditions.
Facet Joint Syndrome
Progressing age causes wear and tear in the structures of the spine. This wear and tear sometimes develops into a condition called facet syndrome, which is one of the most common types of arthritis.
Even though this is commonly seen in the elderly population—usually comprising of adults aged over 50 years—it may also develop in younger people.
However, the causes of the condition in young people are most commonly physical trauma or overuse of the backbone.
Every day, hundreds of Americans deal with these conditions, adopting ways and methods to manage the symptoms with lifestyle changes so that they don’t have to go for surgery.
At Houston Neurosurgery and Spine, we make it a point to get an extensive and thorough history of your health and symptoms before making a diagnosis and moving on to further treatment.
We also use diagnostic imaging and special injections to detect if a facet joint is the cause of pain. If a facet joint is found to be linked to the pain, the patient is referred to an interventional pain physician who can treat the pain using non-surgical methods.
Facet Joint Syndrome: The Causes
Facet joints are small joints, placed between each individual vertebra in the vertebral column. These joints are lined with cartilage, providing the necessary lubrication in order to provide the spine the needed flexibility. This cartilage helps the joints maintain their function of constant motion, allowing us to carry out physical activities like walking, bending, and twisting.
Sometimes, due to injury, overuse or aging, the cartilage inside the facet joint can break down, wear out and cause growths known as ‘bone spurs’ to develop, creating friction in the joints. This friction can lead to a multitude of issues including swelling, tenderness, pain and stiffness.
Damage to the joint like injury, deterioration or any kind of physical trauma may result in swelling, pain and stiffness. The resulting inflammation may be temporary but having arthritis may complicate the situation and lead to long-term or even permanent disability.
There are additional risk factors for the facet syndrome apart from age. These include:
- Obesity
- Overuse of the spinal column in an improper posture for sports or heavy labor
- Having certain medical conditions like gout, arthritis or infections
- Physical trauma like injuries or excessive weight lifting in an improper posture
- Pain that is aggravated in the morning and at night or is affected by climate changes.
- Radiating pain in the lumbar back region that spreads to the shoulders, one or both arms and sometimes even the hands
- Ringing in ears that is accompanied by a headache at the back of the head, the base of the skull or behind the eyes.
- Muscle weakness in limbs
- Lower back pain after standing for a long time
- Pain that worsens on sitting for a long time
Symptoms of facet joint syndrome or axial back pain can be managed and reduced to a great extent without surgical intervention. The degree of relief felt differs from patient to patient and ranges from temporary to significant.
- Physiotherapy that would help support the core muscles and strengthen your back to improve posture.
- Alternating between hot and cold compresses
- NSAID (non-steroidal anti-inflammatory medication, such as ibuprofen) and COX-2 inhibitors (such as Celebrex)
- Lifestyle changes that would help reduce pressure on the muscles at the back
Sometimes, conservative care doesn’t work and the symptoms progress and become chronic.
If this continues for a period of more than six months, surgical intervention or injections may be required to help ease the symptoms. The facet joints connect to the exiting nerve through a small medial branch nerve that connects to the column of muscles in the back. This is the nerve that carries the pain signals from the back to the brain.
A pain management physician can easily diagnose this condition with the help of a series of examinations like a physical check-up, radiographic readings, and finally, a confirmatory facet medial branch block injection. If the pain relief experienced is rated to be higher than 90%, the patient may be recommended a percutaneous radio frequency rhizotomy.
The percutaneous rhizotomy procedure consists of a probe being inserted into the body, guided by an X-ray image, allowing indirect visualization for targeting the medial branch nerve.
Next, the probe is heated to help ablate the small nerve, resulting in instant pain relief.
According to patient reviews, a percutaneous rhizotomy successfully resolves pain related issues in about 70% of patients who opt for it for a year. In some cases, the results may even last up to 5 years. It is up to the patient to choose to be sedated or not, depending on their pain threshold.
When percutaneous radio frequency doesn’t seem to be helping, or the effect fades off too quickly, an endoscopically assisted radio frequency rhizotomy might help. To carry out the procedure, a 7mm tube is inserted into the facet, assisted by X-ray imaging and a working channel endoscope tube attached to an HD camera.
Guided by direct visualization, a physician is able to ablate the medial branch nerve with a radio frequency probe. According to results from clinical literature, around 80% of patients reported a 50% or more reduction in back pain which lasted for up to 5 years. The endoscopic approach has also proven to last longer than radio frequency ablation.
Failed Back Surgery Syndrome
Failed back surgery syndrome, (FBSS) is a term referring to the chronic and severe pain a patient can experience after unsuccessful surgery. FBSS affects up to 40 percent of patients who have had traditional open back or minimally invasive spine surgery. Often surgery is indicated for an identifiable source of pain due to pinched nerve root or an unstable and painful joint. However, back pain can have many causes and accurate identification of the source of pain is complicated. Too often an x-ray and Magnetic resonance imaging (MRI) scans does not correlate well with symptoms. Therefore, diagnostic injections are often warranted and assist in making the proper patient selection and spinal level for surgery.
- Inaccurate diagnose of the condition(s)
- Failure resulting from spine fusion
- Lateral recess stenosis
Failure to decompress the area between the midline and lateral aspect of the exiting nerve - Surgery performed at the wrong level of the spine
- Adjacent segment disease
The development of pain, instability of degenerative conditions at the level above of below the previous surgical site. - Scar tissue formation
- Missed disc fragment, re-herniation of disc or bone spurs still pinching the spinal nerve
- Nerve damage from surgery
What are the symptoms of Failed Back Surgery Syndrome?
The pain associated with failed back syndrome varies depending on the surgical procedure performed and the conditions treated. The pain can range from a dull ache to sharp stabbing pain and may be localized to one area of the back or reach into the legs. Patients suffering from FBSS can experience any of the following symptoms:
- Chronic pain
- Pain at the adjacent area above or below the previous treated area
- Decrease Mobility
- Aching and dull pain in the back, legs or neck
- Sharp or stabbing pain
- Spasms
- Increase dependence of pain medicine
- Medical history
Assessment of symptoms, previous treatments and care. - Physical examination
A careful examination by a spine specialist for limitations of movement, problems with balance, and pain. The examination should also cover loss of reflexes in your extremities, muscle weakness, loss of sensation or signs of spinal cord damage. - Diagnostic tests
Generally, plain x-ray films are taken which allows the physician to rule out other problems such as infections. CT scans and MRIs are often used to give them a three-dimensional view of the lumbar spine and can help detect herniated discs.
What Are The Treatment Options For Failed Back Surgery Syndrome?
Treatment of failed back surgery syndrome and chronic pain is difficult. In order to accurately diagnose FBSS a complete history and symptoms the patient is experiencing. It is also important to get a new MRI or CT Scan and do diagnostic injections to better understand what is causing the pain and pinpoint the affected area.
Surgical Treatment
Once conservative measures have been exhausted and the patient is still in considerable pain after 6 months then minimally invasive procedures may be recommended. The following procedure has shown great results in alleviating pain altogether and returning patients to work and life sooner than traditional spine surgery.
- Transforaminal Endoscopic Discectomy
Treats herniated, bulging, protruded, and extruded discs. Under direct visualization the physician uses the endoscope to decompress the disc to relieve the pressure on the affected spinal nerve. - Endoscopic Foraminalplasty
Treats degenerative disc, foraminal stenosis and facet disease. As the space between the facets diminishes the foramen (natural opening for the spinal and exiting nerves) becomes narrow and begins to compress the nerves. The endoscopic technique uses ronguers, reamers and small motorized burrs to selectively take some bone in order to enlarge the foramen thus decompressing the nerves freeing them up. - Endoscopic Rhizotomy
Patients who have received some temporary relief from percutaneous medial branch rhizotomy but the pain came back are good candidates for endoscopic rhizotomy. This procedure allows the physician to place a small cannula and endoscope inside the patients back and target visually the medial branch nerve. A radiofrequency probe is used through the endoscope to ablate the medial branch nerve. The results of an endoscopic rhizotomy have been significantly better long-term than traditional percutaneous rhizotomy. - Microdiscectomy
Usually an open procedure or using tubular retractor with an incision of 1 inch. The surgeon usually observes through a microscope or set of eyeglass loops that helps magnify the anatomy. Recovery can be long and painful. Most of the pain post-operative is from the approach the surgeon made through major muscle support in your back. Anesthesia is necessary. - Minimally Invasive Discectomy and Fusion
The surgery involves removing the damaged intervertebral disc and replace it with a piece of bone or PEEK cage packed with bone to assist in union or fusion of the two vertebral bodies over time.
Most minimally-invasive patients can begin getting out of bed hours after surgery and go home shortly afterward. With a MIS spine fusion, the time for post-operative recovery is longer and may involve overnight stay in the hospital. Activity is gradually increased and patients are typically able to return to work within a few days to 2 weeks depending on the type of surgery and job description. With a spine fusion return to work may be up to 4-8 weeks. There will probably be some pain after the procedure and is usually localized to the incision site. However, just because there is less or no pain, always consult your physician before beginning any physical work.
At home, you will need to continue to rest. You will be instructed on how to gradually increase your activity. You may still need to take the pain medications for a while. However, pain and discomfort should begin to reduce within a couple of days after surgery. The doctor will discuss with you other techniques for reducing pain and increasing flexibility before you leave for home. The doctor will also discuss with you a time frame for when you can resume basic activities such as walking, driving and light lifting, and when you can return to more advanced activities such as physical labor, sports and yard work.
Foraminal Stenosis
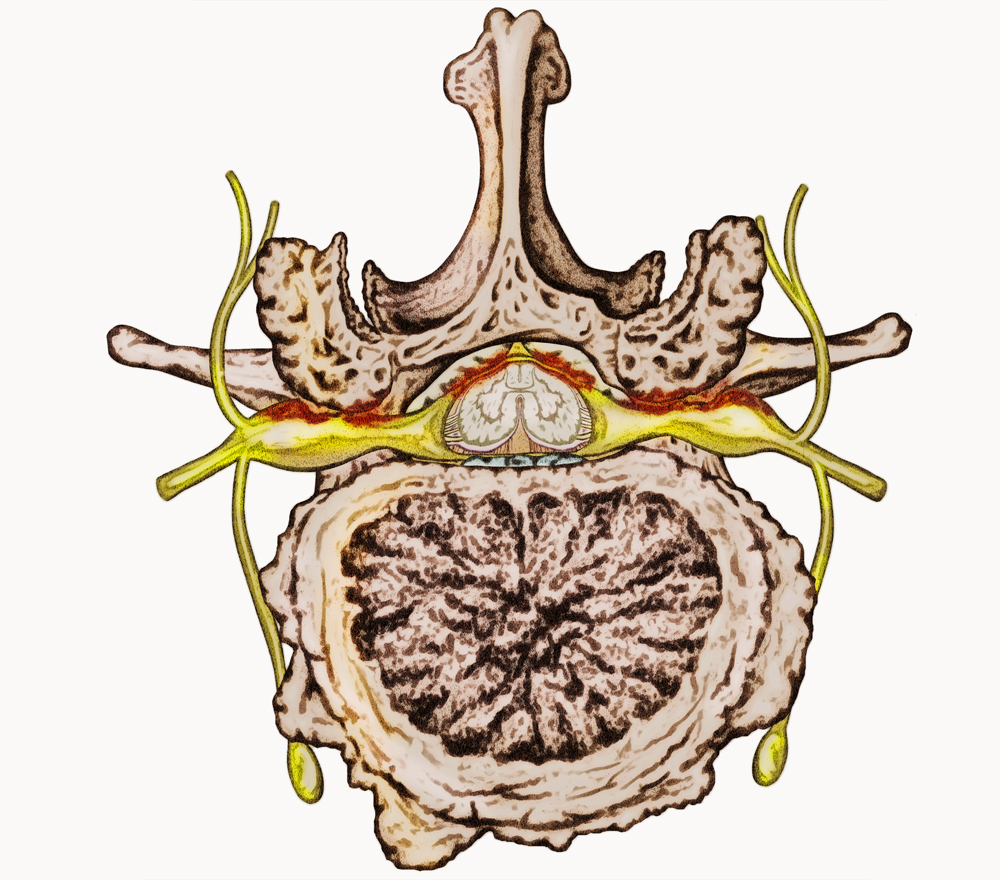 The spine is made up of 33 vertebral bones. Each the bones has a large central canal opening for the spinal cord. Additional openings on each side of the spinal cord called foramens allow the exiting nerves to branch out from the spinal cord to the arms, legs and other parts of the body. The foramen is the space where the exiting nerve exits formed by two facet bones (facet Joint) above and the disc between the vertebral bodies below the exiting nerves.
The spine is made up of 33 vertebral bones. Each the bones has a large central canal opening for the spinal cord. Additional openings on each side of the spinal cord called foramens allow the exiting nerves to branch out from the spinal cord to the arms, legs and other parts of the body. The foramen is the space where the exiting nerve exits formed by two facet bones (facet Joint) above and the disc between the vertebral bodies below the exiting nerves.
What Causes Foraminal Stenosis?
Normally nerve roots have enough room to exit the spinal canal through the foramen. However, with age, degenerative disc disease and trauma, the foramen can narrow and compress the spinal cord and or exiting nerves. Some other conditions such as bulging or herniated discs, calcified ligaments and bone spurs and spinal arthritis may further affect the foramen. This condition can develop anywhere in our spine from cervical to thoracic and is most common in the lumbar region. The average age of patients suffering from spinal and foraminal stenosis is 55 years of age. The disease may affect women and men of varying ages and physical activity levels.
The patients at highest risk for stenosis are:
- Obese
- Smokers
- Sedentary lifestyle
- Lacking proper nutrition
What are the symptoms of Foraminal Stenosis?
Compression on the spinal and exiting nerve leads to inflammation which produces many different types of symptoms depending on the severity of the compression. The symptoms experienced among patients can vary depending on the area of the spine affected or compressed. In the cervical (neck) region, symptoms may be experienced in the neck, shoulders and arms down to the fingers. In the lumbar (back) region, symptoms can be felt in the back, buttocks, thighs, knee, calves, feet and toes. The most common symptoms include:
- Dull, sharp or radiating pain
- Weakness or numbness in the extremities
- Sensation of burning or pins and needles
- Difficulty walking or standing straight
- Medical history
Assessment of symptoms, previous treatments and care. - Physical examination
A careful examination by a spine specialist for limitations of movement, problems with balance, and pain. The examination should also cover loss of reflexes in your extremities, muscle weakness, loss of sensation or signs of spinal cord damage. - Diagnostic tests
Generally, we start with plain x-ray films, which allow us to rule out other problems such as infections. CT scans and MRIs are often used to give us three-dimensional views of the lumbar spine and can help detect Foraminal Stenosis .
Non-Surgical Treatment ?
- Alternating heat/cold therapy during the first 24-48 hours
- Pain medications
Anti-inflammatories, muscle relaxers and on rare occasions narcotic painkillers - Physical therapy exercises to include: stretching, massage strengthening
- Epidural steroid injections are used two-fold, first, to relieve inflammation of the affected spinal nerve and secondly, diagnostically to confirm the correct affected level at which the pain originates from.
Surgical Treatment
When conservative care is exhausted and the patients are still in pain, surgery is a logical step to relieve the pain. Traditionally, central and lateral recess stenosis is performed open with a large incision in the skin. A laminectomy and or facetectomy are performed to release the pressure on the spinal cord. Unfortunately, this technique is invasive and leads to significant post-operative pain and recovery. With innovation and advances in technology, a less invasive surgical technique has been developed to address these painful conditions such as foraminal stenosis.
- Laminectomy
During the microdiscectomy surgeons often have to resect the bone called the lamina in order to see the affected nerve and herniated disc. Recovery from microdiscectomy can be long and with bone, resection adds to possible scarring in the area the surgeon is working. Anesthesia is necessary. - Endoscopic Foraminalplasty
Unlike traditional surgery, a small ¼ inch incision is made in the skin. Your muscles are spared and only dilated in order to gain access to the surgical site. The physician uses a working channel endoscope that allows for water and instruments to pass through the scope with an HD camera attached hat provides a superior view of the anatomy and the spinal cord. The patient is under conscious sedation alert and comfortable throughout the procedure. No general anesthesia is needed and thus lower risk to the patient. - Spinal Fusion
Spinal fusion surgery is designed to stop the motion at a painful vertebral segment, which in turn should decrease pain generated from the joint. Spine fusion when indicated should be the last options offered but can be performed effectively with advanced MIS techniques. Sometimes when patients suffer from foraminal stenosis that fails a laminectomy or facetectomy are often left with instability and MIS fusion is appropriate to provide stability and further decompress the foramen and spinal nerve.
What Is The Recovery ?
Most patients can begin getting out of bed one hour after surgery and go home shortly afterward. Activity is gradually increased and patients are typically able to return to work within a few days. There will probably be some pain after the procedure and is usually localized to the incision site. However, always consult your physician before beginning any physical work.
Always seek your physician’s opinion when it is safe to return to work. Also, light administrative duty is recommended until your physician approves of any physical demands at your place of work.
At home, you will need to continue to rest. You will be instructed on how to gradually increase your activity. You may still need to take the pain medications for a while. However, pain and discomfort should begin to reduce within a couple of days after surgery. We will discuss with you other techniques for reducing pain and increasing flexibility before you leave for home. We will also discuss with you a time frame for when you can resume basic activities such as walking, driving and light lifting, and when you can return to more advanced activities such as physical labor, sports, and yard work.
Herniated Disc
Lumbar Disc Herniation
Time and age can exert a lot of pressure on the spine and its discs. In most cases, herniated discs care caused by sustaining trauma or an injury—for example, an accident—that directly exerts pressure on the disc.
Slowly, over time, the outer bone of the spinal column—called the annulus—cracks and develops tears, causing the gel-like nucleus inside to push out through the tear. This is called a bulging disc.
Bulging discs exert stress on the spinal cord (dura) and the nerve roots that exit through the foramen, extending to the lower limbs and muscles. Symptoms of bulging discs are not always felt.
In case of a weak or brittle annulus, the tears can cause the inner nucleus to protrude (resulting in a ruptured disc) or extrude (resulting in a herniated disc).
Sometimes, the nucleus even leaks fluid and leaves the disc entirely resulting in a condition called a sequestered disc. If left untreated, a herniated disc can progress and increase the pressure exerted on the spinal nerves. This causes inflammation and the resulting pain can either be localized to the lumbar back region or extend down to the limbs and feet.
A herniated disc in the lumbar region is the most common cause of pain the lower back and limbs. Lumbar discs consist of annulus fibrosis, which looks like an interwoven fabric, and the gel-like nucleus pulposus. Placed at each level of the vertebral column, these discs act as shock absorbers.
Herniated Discs: Its Causes
As we age, our spine and discs deal with additional pressure. Most cases of herniated discs stem from experiencing serious physical trauma—for example, an accident—that causes direct pressure in the area the disc is located.
If this compression is left untreated, over time, the annulus will start to develop cracks and tears, causing the inner nucleus to be pushed out and leak fluid through the disc.
This pushing out of the nucleus exerts causes stress to the spinal cord and puts pressure on the nerve roots exiting through the foramen (holes at each level of the vertebral column) and connect with the muscles traveling down your leg.
The pressure exerted combined with the fluid leakage of the nucleus results in inflammation and the resulting pain may most commonly be localized to the back, buttocks, thighs; other times, it may also travel down and extend to the feet.
Risk factors associated with herniated discs are listed in the following:
Aging:
Age causes the discs to wear out and get dry over time, resulting in loss of support and function.
Lifestyle:
Poor lifestyle choices like smoking, lack of a balanced diet, not exercising enough, and obesity attribute to a higher risk of disc degeneration.
Posture:
Maintaining a poor posture when lifting or moving around exerts direct stress and pressure on the spinal and discs.
In the event of conservative treatment failing, the patient will be required to undergo diagnostic tests like CT scans or MRI.
If a neurological deficit is detected, surgical intervention will be recommended. Following are the best surgical treatment options for herniated discs with a success rate of 90%:
- A dull, sharp pain the lumbar regions of the back that worsens with certain physical activities that include lifting heavy objects and bending awkwardly. The pain can also get worse with simple activities like sneezing and conditions like muscle spasms or experiencing muscle cramps.
- Having a condition called sciatica or its symptoms are also often signs of a herniated disc.
- Weakness or loss of function of the leg
Diagnosis
The first step to coming up with an effective treatment plan is a correct and accurate diagnosis.
Here are some of the most effective ways to diagnose the problem areas.
Medical History:
This involves a certified doctor going through a patient’s previous medical and treatment history and assessing symptoms.
Physical Examination:
A spine specialist physically carries out routine spine examination steps to check for problem areas like limitation of movement, balance problems and pain. A thorough spine examination also covers loss of reflexes in extreme regions, weakness in the muscles, loss of sensation or any signs of damage in the spinal cord.
Diagnostic Tests:
This step generally begins with a plain X-ray which helps spine specialists rule out some problems like infections, if required, CT scans and MRIs are then ordered to provide a more detailed three-dimensional view of the lumbar spine which helps detect the presence of herniated discs.
Treatment Options
Disc herniation in the lower spine typically does not warrant surgery. Most often, any pain that stems from a herniated disc heals on its own within 4–6 months without surgical intervention, which is why as a first step, non-surgical treatments are advised to help deal with the symptoms and pain.
Non-Operative Treatment
- Pain meds: anti-inflammatory medication, muscle relaxers and rarely, narcotic painkillers may also be prescribed.
- Administering heat/cold therapy, alternatively, in the first 24–48 hours.
- Helpful and light physical therapy including exercises like stretching, massage strengthening.
- Epidural steroid injections that work to reduce inflammation and determine the level at which the individual experiences pain.
Surgical Treatment for Disc Herniation
In case non-operative treatment doesn’t work and the symptoms persist, the patient is sent for further diagnostic tests like CT scan, MRI or X-ray to identify defects, problem areas or neurological issues.
In case a problem worthy of surgical treatment is detected, the patient is recommended surgical solutions.
In the following are surgical treatment options for the treatment of herniated discs with a success rate of 90%
Microdiscectomy:
This is generally an open procedure where a tubular retractor is used to make an incision of around 1 inch. This is done under anesthesia.
During the procedure, the surgeon uses a microscope or eyeglass loops to observe the area being treated. This procedure has a longer recovery time and the patient might experience some pain from time to time. Most of the pain will come post-operation and is the result of the approach of treatment.
Laminectomy:
Also known as decompression surgery, this process is used to create space for the removal of pressure on a nerve by removing the lamina, the back part of the vertebra, covering the spinal canal.
This procedure is sometimes carried out along with microdiscectomy, and increases the chances of scarring in the area being treated. It also adds to the recovery time.
Endoscopic Discectomy:
This procedure requires an incision of less than half an inch. The process of endoscopic discectomy makes it possible for the surgeon to avoid resection of the lamina bone for entering the spinal canal. It makes it easier to enter the spinal canal without causing major damage including the cutting or disturbing of muscles.
During the procedure, the surgeon is able to observe the herniated disc directly in a water environment (arthroscopy).
To perform the process, a surgical working channel endoscope is used with an HD camera. This procedure requires a comparatively lower recovery time than microdiscectomy, and in most cases, patients are able to return to work in less than a week.
Spinal Fusion
Usually, spine fusion is seen as a last resort for patients displaying symptoms of discogenic back pain or herniated discs.
The process of endoscopic discectomy allows physicians to detect the affected disc while the patient is under conscious sedation.
The procedure involves making an incision of around ¼ of an inch and placing a 7 mm working cannula into the foramen. This insertion is usually done from the side to avoid causing any major damage to the surrounding muscles or tissues.
An HD camera is then guided into the working channel endoscope to help the physician carry out the procedure accurately.
Recovery
At our practice, many patients who undergo spinal fusion will be able to get out of bed in just over an hour of the having the procedure performed and will be able to go home shortly afterward.
There is some pain, localized to the incision site, that will be felt from time to time for a few days, post-surgery, but despite that fact, most people will feel well enough to return to work in a few days. Till then, pain killers will be provided to ease the post-op symptoms.
Once you’re done with the procedure, plenty of rest is recommended to speed up the healing process. The doctors will make sure to provide you with ample guidance on how to care of your area of incision and gradually increase physical activity to not set back the recovery time and avoid any further damage to the area of treatment.
The pain and discomfort will begin to heal in a couple of days post-surgery and patients will be instructed to use adequate medication and techniques for reducing pain and increasing flexibility.
The patient will also be given a time frame to indicate when and how to resume daily activities such as walking, lifting weight and driving and the optimal time frame of returning to activities like physical labor work or sports.
Low Back Pain

What Causes Lower Back Pain
n most cases, lower back pain stems from mechanical causes. Pain in the lower region of the back occurs due to a condition called Spondylosis which refers to the degenerative changes that occur in the spine such the wear and tear of the joints, bone spurs and the degeneration of the intervertebral discs.
Some common mechanical causes of lower back pain include:
Muscle sprains and strains:
A sprain occurs when you overstretch or accidentally tear a ligament, while strains refer to tears in the tendon or muscle. Both conditions can stem from movements like twisting, overstretching, or lifting something heavy with an improper posture.
Sometimes, these movements can also lead to painful spasms in the back muscles. Generally, muscle strains indicate the presence of acute back pain, but if not taken care of, the condition can progress into a facet joint syndrome.
Degenerative Disc Disease:
Characterized by pain caused by damaged, dehydrated or deteriorated vertebral discs because of a degenerative disease.
Disc degeneration, in its early stages, may not cause symptoms like severe pain, but as the disease advances, you may experience pain in the lower back..
Herniated or Ruptured Discs:
As humans age, their intervertebral discs may get compressed and bulge outward. This is called herniation, and can cause the lower back region to become very painful. These herniated discs may also rupture, which also results in lower back pain.
Radiculopathy:
Sometimes, a spinal nerve root can become compressed or inflamed, resulting in symptoms like pain or numbness that may also radiate to various other parts of the body that are connected to that particular nerve.
Other conditions like spinal stenosis, herniated or ruptured discs may also compress nerve roots, leading to radiculopathy.
Sciatica:
This is a form of radiculopathy caused by the compression of the sciatic nerve.
The sciatic nerve is a large nerve in the body that starts in the lower back, splits above the hip and runs all the way down to the back of the legs.
When the sciatic nerve is compressed, it causes shock-like or burning pain in the lower back that is often paired with pain in the buttocks and legs, sometimes even reaching the foot.
Spondylolisthesis:
Sometimes, a vertebra at the base of the spine slips out of its own place and pinches the nerves connected to the spinal cord, causing pain in the lower back.
Traumatic Injury:
Actions like playing sports, car accidents or experiencing a fall may cause serious damage to the ligaments, muscles or tendons which can lead to pain in the lower back region.
Traumatic injuries can also exert extra pressure on the spine which can lead to rupturing or herniation of the intervertebral disc. This can further compress the nerves rooted in the spinal cord, resulting in back pain or even sciatica.
Spinal Stenosis:
This is a common condition that occurs as a result of the spinal column narrowing down. This exerts pressure on the spinal cord and the nerves connected to it. This causes symptoms like numbness with walking and if not taken care of, may lead to weakness in the leg and even sensory loss.
Scoliosis:
A sideways curve in the spine that mostly develops right before puberty and generally isn’t painful in its early stages or up until the middle age.
Lordosis is the abnormal inward curvature in the lower back region. In a lot of cases, scoliosis can lead to chronic pain that may require surgery in order to help heal.
Here are the most common symptoms of lower back pain.
- Pain in lumbar disc tear region. This pain usually travels into the buttocks and thighs but doesn’t go past the knees.
- Lower back and buttock muscle spasms
- Problems related to disc tears or bulging and herniated discs may result in numbness or tightness in the region. Bulging outwards, or herniation of the disc can also lead to numbness in the legs
- Weakness in the buttocks, thighs, or temporary loss of leg control may occur from a spinal nerve being compressed or irritated.
- A tingling sensation in the legs or feet may be caused as a result of degenerative disc disease, annular tears, spinal stenosis or herniated discs.
What Are The Treatment Options For Low Back Pain?
Treatment for low back pain ranges from conservative therapies to surgical intervention. The goals of treatment are to relieve pain, prevent or reduce stress on the discs or spinal nerves and maintain normal function. It is always recommended that patient be prescribed non-surgical conservative treatment initially to help relieve symptoms.
Non-Operative Treatment
- Alternating heat/cold therapy during the first 24-48 hours
- Pain medications
anti-inflammatories,muscle relaxers and on rare occasions narcotic painkillers - Physical therapy exercises
stretching, massage strengthening - Transforaminal Epidural Steroid Injections
are used two-fold, first, to relieve inflammation of the affected spinal nerve and secondly, diagnostically to confirm the correct affected level at which the pain originates from - Facet Joint Injections/Medial Branch Nerves
can provide immediate short-term relief from painful symptoms and provide a diagnostic result confirming the affected level where the pain originates in the patients low back. - Discography
a diagnostic injection technique used to determine which discs of a patient’s spine, are a source of pain. - Platelet Rich Plasma Injection (PRP)
Blood platelets play an activation role in your body’s wound and soft tissue healing. The patient’s own blood, having platelets, is concentrated down through the use of a special machine called a centrifuge. These PRP can be used to promote healing of injured ligaments, tendons, muscles and joints.
Surgical Treatment
Once conservative measures have been exhausted and the patient is still in considerable pain after 6 months then minimally invasive procedures may be recommended. The following procedure has shown great results in alleviating pain altogether and returning patients to work and life sooner than traditional spine surgery.
- Endoscopic Discectomy, Annuloplasty
A ¼ inch incision is made and a 7mm operating tube is placed on the disc at the site of the annular tear. An endoscope with HD camera is inserted into the operating tube to visualize the annulus and spinal nerves. Then the tear is debrided to make sure no nucleus pulposus is stuck within the annulus and thermally heated with a bipolar instrument to reduce and close the tear. - Endoscopic Rhizotomy
A least invasive procedure done outpatient to help patients suffering from chronic back pain and muscle spasms. Patients who have received some temporary relief from percutaneous medial branch rhizotomy, but the pain came back are good candidates for endoscopic rhizotomy. - Minimally Invasive TLIF
- Endoscopic Surgery
Most endoscopic patients can begin getting out of bed one hour after the procedure and go home shortly afterwards. There will probably be some pain after the procedure and is usually localized to the incision site. However, just because there is less or no pain, always consult your physician before beginning any physical work. Patients can return to administrative work within a week. No physical activities including work are recommended for 6 weeks. - Minimally Invasive Spine Surgery
At home, you will need to continue to rest. You will be instructed on how to gradually increase your activity. You may still need to take the pain medications for a while. However, pain and discomfort should begin to reduce within a couple of days after surgery. The doctor will discuss with you other techniques for reducing pain and increasing flexibility before you leave for home. The doctor will also discuss with you a time frame for when you can resume basic activities such as walking, driving and light lifting, and when you can return to more advanced activities such as physical labor, sports and yard work. Most patient can return to work within a few days.
Neck Pain Center
What You Need to Know About Neck Pain
Neck pain can be caused by any number of conditions from poor posture, injury, herniated  cervical disc, or strains.
cervical disc, or strains.
Neck pain affects the flexibility of your body, reducing your range of movement. Without proper care, the pain can progress and worsen over time and may radiate down your back and spread to other parts of your body.
Some causes of neck pain include:
- Sports injury – especially contact sports
- Poor posture in general
- Craning your neck
- Hunching over a desk all day
- Sustaining trauma or injury such as whiplash
- Neck strain
- Cervical radiculopathy
- Cervical spondylosis
Behaviors that distort the natural alignment of your neck like sitting at a computer too long, falling asleep in a sitting position or carrying heavy objects on your shoulder cab cause pain in your neck.
Neck And Spine Pain Center In Houston
If you’re experiencing any of these symptoms in Houston, schedule an appointment with Dr. G. Alexander West, one of the most recognized top neurosurgeons in the United States. As the resident doctor in our neck and spine center, he specializes in every kind of back and neck pain including cervical pain and other conditions. His expertise in micro-neurosurgery, back-disc surgery and spine surgery, and other non-invasive and minimally-invasive procedures can help relieve severe pain in the neck, back and shoulder, back of the head and muscles.
Schedule an appointment today to get started.
Pinched Nerve
WBulging Disc and Pinched Nerve
The spinal cord act as a communication carrier. It carries messages from the brain to the rest of the body and back too.
The spinal cord extends down the vertebra, with nerve cells branching out and connecting with the muscles everywhere in the body. Sometimes, these nerves become pinches, either because of bulging or herniated discs, or growths called bone spurs.
When this happens, your body sends pain signals to your brain. These signals should never be ignored. Damage occurring because of a compressed nerve can be minor but if proper treatment is not sought soon, it may progress into major damage and can result in temporary or even permanent health issues and pain. It is best to seek help from an experienced spine specialist as soon as you can in order to get your symptoms diagnosed properly and get started on an effective treatment plan.
In some cases, if a pinched nerve goes untreated for a long time, it may result in permanent damage such as sensation loss in the affected area or muscle weakness.
Causes of Pinched Nerves
Spinal and exiting nerves pass through narrow holes in the vertebral column, called the foramen. These nerves are the most vulnerable in your spinal canal. Sometimes, a tendon, disc or the surrounding bony structures can exert pressure on one of these nerves, ‘pinching’ them. This pinching often happens due to the degeneration of the spine over time, or in some cases, because of some physical trauma, like an injury or an accident.
There are some other activities that may also cause spinal or disc degeneration and lead to a compressed or pinched nerve such as maintaining a poor posture, lifting heavy objects improperly and repetitive motion.
When a nerve is compressed or becomes ‘pinched’, an inflammatory process starts immediately, resulting in pain in the neck or lumbar regions of the back.
Sometimes, this pain can spread and reach your shoulder and travel down the arm (cervical radiculopathy), or even radiate down the leg and cause a condition known as sciatica.
Age or physical trauma, like an accident, for example can cause the discs that lie between the vertebrae to become weak and develop cracks or tears. This causes the nucleus pulpous—the inner part of the disc—to push out through the annulus, which is the outer part of the disc outward, resulting in a bulging structure, called a bulging or herniated disc that exerts pressure on the spinal cord and may cause pain.
Symptoms of Pinched Nerves
A tingling sensation accompanies by numbness is often the most common symptom of a pinched nerve. Pain may accompany the tingling sensation and is often described as being “sharp” or “electrical”. Some patients experience a burning or tightness sensation in the affected area.
If the case is more severe, the pain and numbness can also be accompanied by muscle weakness. This happens when the nerves that control muscle function have been affected.
If this condition is not treated as soon as possible, these muscles may start to deteriorate in size, become weaker and lose their function.
If treatment for nerve compression is not started immediately, the damage can spread to the protected area around the nerve and cause swelling and scarring. This condition can result in peripheral neuropathy, carpal canal syndrome and excruciating pain in the arm.
- Medical history
Assessment of symptoms, previous treatments and care. - Physical examination
A careful examination by a spine specialist for limitations of movement, problems with balance, and pain. The examination should also cover loss of reflexes in your extremities, muscle weakness, loss of sensation or signs of spinal cord damage. - Diagnostic tests
Generally, we start with plain x-ray films, which allow us to rule out other problems such as infections. CT scans and MRIs are often used to give us three-dimensional views of the lumbar spine and can help detect Pinched Nerve.
Non-Surgical Treatment ?
- Alternating heat/cold therapy during the first 24-48 hours
- Pain medications
Anti-inflammatories, NSAIDS, muscle relaxers and on rare occasions narcotic painkillers - Physical therapy exercises to include: stretching, massage strengthening
- Epidural steroid injections are used two-fold, first, to relieve inflammation of the affected spinal nerve and secondly, diagnostically to confirm the correct affected level at which the pain originates from.
Surgical Treatment
If pain still persists and patient is intolerant to the pain after non-surgical treatment and there is evidence by CT Scan, MRI or X-ray or neurological deficit, then surgical intervention is usually recommended. The following surgical options can treat bulging disc and pinched nerves with 90% success:
- Microdiscectomy
Usually an open procedure or using tubular retractor with an incision of 1 inch. The surgeon usually observes through a microscope or set of eyeglass loops that helps magnify the anatomy. Recovery can be long and painful. Most of the pain post-operative is from the approach the surgeon made through major muscle support in your back. Anesthesia is necessary. - Laminectomy
During the microdiscectomy surgeons often have to resect the bone called the lamina in order to see the affected nerve and herniated disc. Recovery from microdiscectomy can be long and with bone resection adds to possible scarring in the area the surgeon is working. Anesthesia is necessary. - Spinal Fusion
A spinal fusion surgery is designed to stop the motion at a painful vertebral segment, which in turn should decrease pain generated from the joint. Spine fusion when indicated should be the last options offered. Sometimes when patients suffer from discogenic back pain, recurrent herniated disc and or instability and have failed less conservative surgical options, a spinal fusion may be indicated.
What Is The Recovery ?
Most patients can begin getting out of bed one hour after surgery and go home shortly afterward. Activity is gradually increased and patients are typically able to return to work within a few days. There will probably be some pain after the procedure and is usually localized to the incision site. However, always consult your physician before beginning any physical work.
Always seek your physician’s opinion when it is safe to return to work. Also, light administrative duty is recommended until your physician approves of any physical demands at your place of work.
At home, you will need to continue to rest. You will be instructed on how to gradually increase your activity. You may still need to take the pain medications for a while. However, pain and discomfort should begin to reduce within a couple of days after surgery. We will discuss with you other techniques for reducing pain and increasing flexibility before you leave for home. We will also discuss with you a time frame for when you can resume basic activities such as walking, driving and light lifting, and when you can return to more advanced activities such as physical labor, sports, and yard work.
Sciatica
When experiencing symptoms of sciatica or sciatic pain, it is recommended to understand it before starting treatment.
Symptoms of sciatica are generally associated with pinched or compressed nerve roots that are connected to the spinal cord. As the spinal column runs down from the base of the skull to right above the hip, nerves exit through the foramen (tiny holes on either side of the spinal bone) at each level of the spine. These are called radicular nerves or nerve roots. Beginning from the nerve roots in the lumbar spinal cord, the sciatic nerve extends onwards through the buttocks and down the limbs.
Sciatica can occur in both the left and right legs. This type of pain is also called radicular pain or radiculitis (inflammation of the nerve root). Radicular pain often occurs as a result of a compressed or inflamed spinal nerve. This type of pain sits deep and often worsens with certain activities like standing, walking or even sitting.
walking or sitting. Documented nerve dysfunction condition is referred to radiculopathy.
- Cramping in muscles
- Burning sensation
- Numbness in the affected area
- Tightness in the affected area
- Weakness in muscles
Treatment Options
In case you’re experiencing on or more of the mentioned symptoms, it is advisable to consult a medical professional as soon as possible. If you’ve tried conservative treatment methods like physical therapy and non-steroidal anti-inflammatory (NSAIDS) exercise strengthening for six months or more, but your pain still persists, surgical intervention may be prescribed.
In such cases an MRI or CT scan may also be required in order to proceed with further treatment.
At Houston Neurosurgery and Spine, we offer the following treatment options for Sciatica:
Endoscopic Discectomy:
This is, to date, least invasive and requires the smallest incision to be made in the spine during surgery. The surgery is carried out under conscious sedation.
An HD camera is paired with an endoscope and is used to surgical visualize and remove any bulging or herniation found in the disc material which is compressing the nerve root. This procedure greatly reduces post-operation pain and the time needed to recover.
Endoscopic Foraminotomy:
This is a minimally invasive procedure that is used to decompress the area around the nerves experiencing pressure in order to open a narrowed spinal canal and relieve pain symptoms.
The endoscopic technique is used along with special tools such as laser, rongeurs, motorized diamond burrs reamers and kerrisons to carry out the procedure.
The Anatomy Of Sciatica
Symptoms of Sciatica, or sciatic nerve pain, is caused by the ‘pinching’ of the sciatic nerve root in the spinal cord.
The spinal cord begins at the base of the skull and travels down the vertebral column passing through the cervical region, thoracic region and the lower back.
The vertebral column contains holes at either side of the spine called the foramen, where a pair of spinal nerves, called nerve roots or radicular nerves, exit at each level.
The sciatic nerve splits in the back, right above the hip and runs down on each leg, connecting with the muscles and tendons in the hip, buttocks, thighs, knees, calves and feet. Even though it is more common to experience sciatic pain in one leg, it may be present in both. This type of pain may also be referred to as radicular pain or radiculitis (inflammation of the nerve root).
Radicular pain occurs when a spinal nerve root is compressed or inflamed. This pain is often described to be deep and steady, and worsen with certain physical activities and positions such as walking, standing for a long time or sitting.
Once diagnosed, a nerve dysfunction is referred to as radiculopathy, by a specialist. There are treatments available for sciatica nerve pain. You can contact us to make your appointment today and learn more about sciatica treatment options.
Spondylolisthesis
The term spondylolisthesis is derived from two Greek words put together; spondylos, which means “spine or vertebra”, and “listhesis”, which means to “slip or slide”.
Spondylolisthesis is a spine condition that develops when a vertebra in your spinal column slips out of its place or gets misaligned.
In case a vertebra slips or slides out too far, direct pressure could fall on one of the spinal nerves and result in pain in the lumbar regions of the back, and weakness in the legs that may also be accompanied by a numbing sensation.
In some rare cases, patients also experience severe symptoms like bladder and bowel control. It is important to seek professional medical care immediately if any of these symptoms become apparent.
What Causes Spondylolisthesis?
The human vertebral column consists of the vertebrae, joined together one on top of the other by small joints on either side, called the facets.
These facets support the spinal functional and allow for smooth movement like bending, twisting and turning. Weakening and degeneration of these joints result in Spondylolisthesis. This condition may develop due to several different reasons, some of them include:
- Presence of a defective facet joint since birth (also known as congenital)
- Damaged or trauma caused to a facet joint
- Overusing the facet joint
- Arthritis or infection
Teenagers and young adults involved in vigorous physical activities like high impact sports are also at the risk of developing the condition.
Overuse and high impact activities can lead to the exertion of extra stress and pressure on the backbone and cause fractures in the vertebrae, resulting in Spondylolisthesis. In the older population, natural wear and tear of the bones and joints are generally the cause behind these fractures.
Although fractures are a serious cause of spondylolisthesis, it is not necessary for them to be present for the condition to develop. Problems like the weakening of the ligaments connecting the vertebrae together can also allow slippage and lead to spondylolisthesis.
The progress of the condition is represented by grades according to how much one vertebra slips in comparison to the other. The grades are defined in the following:
- Grade I – <25%
- Grade II – 25–50%
- Grade III – 50–75%
- Grade IV – >75%
- Grade V – One vertebra has fallen off the next, completely
Symptoms of Spondylolisthesis
Even though it is not unusual for a person with Spondylolisthesis to never experience any symptoms, the most common ones include:
- Pain that starts in the lower back and radiates down one or both legs.
- A numbing sensation or muscle weakness in one or both legs
- Difficulty in walking
- Pain in the lumbar back or buttock region that worsens with certain physical activities such as bending or twisting
- Loss of bladder or bowel control.
Spondylolisthesis: Its Diagnosis and Treatment
Getting started with treatment usually involves cutting down on or stopping any physical activities which may have led to the condition.
This first step is accompanied by anti-inflammatory medication for example ibuprofen to help manage the pain and help the inflammation.
The next step of the treatment plan is usually physical therapy guided by a professional therapist.
The physical therapy routines recommended for the treatment of spondylolisthesis include exercises that strengthen the core, the abdomen and muscles in the lumbar back region and helps build stability in order to avoid chances of further damage.
In case the patient is obese or overweight, a good option to consider would be to focus on weight loss.
If the slippage continues to worsen or the pain persists, surgery is usually recommended. Endoscopic procedures can help decompress the facet joints and central areas of the lamina bones to relieve the pain associated with it.
Here are some benefits of endoscopic surgery:
- ¼ inch incision
- Conscious sedation
- Return to work sooner than minimally invasive or traditional spine surgery
- Minimal recovery time
When there is no need for Endoscopic surgery and the patient’s condition continues to deteriorate, traditional laminectomy may be used to decompress. In certain cases, a fusion may be used to stabilize the facet joint and vertebrae.
Post-surgery, the patient will be asked to wear a back brace for some time to assist with the recovery phase. They may also have to refrain from carrying heavy items.
Rehabilitation therapy is imperative to strengthen the core abdominal and back muscles.